Physical inactivity in people with diabetes in low-income rural areas and associated factors: Amazonas results
DOI:
https://doi.org/10.12820/rbafs.30e0399Keywords:
Physical activity, Type 2 diabetes mellitus, Primary Health Care, Rural areasAbstract
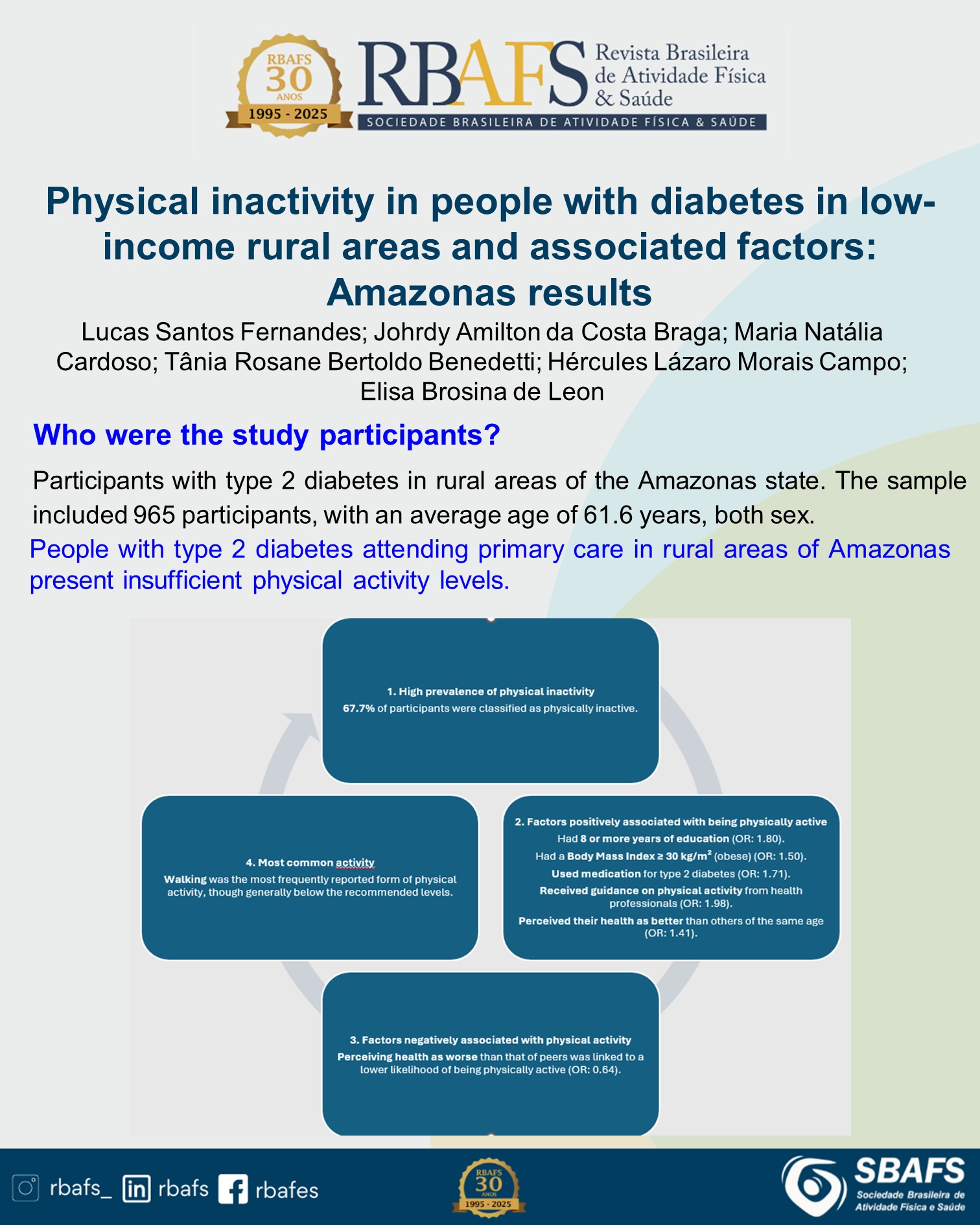
Physical activity (PA) is crucial for the management of type 2 diabetes mellitus (T2DM), but there is a paucity of research on adherence to PA guidelines, PA level, and associated factors in patients with T2DM living in remote areas. Objectives: To investigate adherence to PA, describe PA level, and identify associated factors among patients with T2DM treated in primary health care in Amazonas, Brazil. Methods: This is a descriptive cross-sectional study. Data were collected between 2020 and 2023, with patients from primary health care units in rural Amazonas. The PA level was assessed using the International Physical Activity Questionnaire, along with additional questionnaires on sociodemographic and clinical variables. A significance level of 5% was applied in all analyses. Results: The study included 965 participants, of whom 67.7% were classified as inactive and 80.5% did not meet PA recommendations. Factors positively associated with higher PA level included having ≥8 years of education (OR = 1.80; 95% CI: 1.31 - 2.48), body mass index (≥30 kg/m² (OR = 1.50; 95% CI: 1.04 - 2.17), adherence to prescribed medications (OR = 1.71; 95% CI: 1.15 - 2.54), receiving guidance on PA (OR = 1.98; 95% CI: 1.49 - 2.64) and a positive self-perception of health (OR = 1.41; 95% CI: 1.00 - 1.98). Conclusion: Better PA level was associated with higher education, obesity, medication adherence, PA orientation, and positive health perceptions. These findings highlight the importance of addressing multiple factors to promote PA among patients with T2DM in rural Amazonas.
Downloads
References
1. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077–e1086.
2. Brasil, Ministério da Saúde, Secretaria de Vigilância em Saúde e Ambiente, Departamento de Análise Epidemiológica e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2023: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2023. 1st ed. Brasília: 2023.
3. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde e Ambiente. Departamento de Análise Epidemiológica e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2006-2023: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica do estado nutricional e consumo alimentar nas capitais dos 26 estados brasileiros e no Distrito Federal entre 2006 e 2023: estado nutricional e consumo alimentar / Ministério da Saúde, Secretaria de Vigilância em Saúde e Ambiente, Departamento de Análise Epidemiológica e Vigilância de Doenças não Transmissíveis. – Brasília: Ministério da Saúde, 2024. 80 p.
4. Dempsey P, Friedenreich C, Leitzmann M, Bruman M, Lambert E, Willumsen J. Global public health guidelines on physical activity and sedentary behavior for people living with chronic conditions: a call to action. J Phys Act Health. 2021;18(1):76–85.
5. Coelho-Ravagnani CF, Sandreschi PF, Piola TS, Santos L, Santos DL, Mazo GZ, et al. Atividade física para idosos: Guia de Atividade Física para a População Brasileira. Rev Bras Ativ Fís. 2021;26:0216.
6. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843.
7. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Secretaria de Gestão Estratégica e Participativa. Vigitel Brasil 2008: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico / Ministério da Saúde, Secretaria de Vigilância em Saúde, Secretaria de Gestão Estratégica e Participativa. – Brasília: Ministério da Saúde, 2009.554 p.: il. – (Série G. Estatística e Informação em Saúde)
8. Martin CG, Pomares ML, Muratore CM, Avila PJ, Apoloni SB, Rodríguez M, et al. Level of physical activity and barriers to exercise in adults with type 2 diabetes. AIMS Public Health. 2021;8(2):229–39.
9. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee; Sigal RJ, Armstrong MJ, Colby P, Kenny GP, Plotnikoff RC, et al. Physical Activity and Diabetes. Can J Diabetes 2013;37 Suppl 1:S40-4.
10. American Diabetes Association Professional Practice Committee; 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45(Supplement_1):S60-S82.
11. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behavior. Br J Sports Med. 2020;54(24):1451–62.
12. Brasil. Ministério da Saúde. Secretaria de Atenção Primária à Saúde. Departamento de Promoção da Saúde. Guia de Atividade Física para a População Brasileira / Ministério da Saúde, Secretaria de Atenção Primária à Saúde, Departamento de Promoção da Saúde. – Brasília: Ministério da Saúde, 2021. 54 p.
13. Bertoluci MC, Forti AC, Pititto BA, Vancea DMM, Malerbi FEK, Valente F, et al. Diretriz Oficial da Sociedade Brasileira de Diabetes. Diretriz Oficial da Sociedade Brasileira de Diabetes. 2022 Feb 4. Available from: https://diretriz.diabetes.org.br/2022/ [2024 January].
14. Brasil, Ministério da Saúde M. Protocolo Clínico e Diretrizes Terapêuticas do Diabete Melito Tipo 2. Portaria SCTIE/MS no 54, de 11 de novembro de 2020. Secretaria de Ciência, Tecnologia, Inovação e Insumos Estratégicos. 2020 119. Available from: https://www.gov.br/conitec/pt-br/midias/protocolos/20201113_pcdt_diabete_melito_tipo_2_29_10_2020_final.pdf/view [2024 January].
15. Seidu S, Cos X, Brunton S, Harris SB, Jansson SPO, Mata-Cases M, et al. 2022 update to the position statement by Primary Care Diabetes Europe: a disease state approach to the pharmacological management of type 2 diabetes in primary care. Prim Care Diabetes. 2022;16(2):223–44.
16. Leon E, Fernandes L, Campos H, Almeida F. Management and prevention of diabetes in primary health care in Amazonas. Rev Bras Ativ Fis. 2022;27:1–13.
17. IBGE. Instituto Brasileiro de Geografia e Estatística. Amazonas. 2022. Available from: <https://www.ibge.gov.br/cidades-e-estados/am.html> [2024 January].
18. IBGE. Instituto Brasileiro de Geografia e Estatística. Amazônia Legal. 2022. Available from: <https://www.ibge.gov.br/geociencias/organizacao-do-territorio/estrutura-territorial/15819-amazonia-legal.html> [2024 January].
19. Guimarães AF, Barbosa VLM, Silva MP, Portugal JKA, Reis MHSS, Gama ASM. Access to health services for riverside residents in a municipality in Amazonas State, Brazil. Rev Pan-Amaz Saúde. 2020;11:e202000178.
20. American Diabetes Association; 5. Facilitating behavior change and well-being to improve health outcomes: Standards of medical care in diabetes−2021. Diabetes Care. 2021;44(Supplement_1):S53–S72.
21. Leon EB, Campos HLM, Brito FA, Almeida FA. Study of Health in Primary Care of the Amazonas Population: Protocol for an Observational Study on Diabetes Management in Brazil. JMIR Res Protoc. 2022;11(9):e37572.
22. Apolinario D, Lichtenthaler DG, Magaldi RM, et al. Using temporal orientation, category fluency, and word recall for detecting cognitive impairment: The 10-point cognitive screener (10-CS). Int J Geriatr Psychiatry. 2016;31(1):4–12.
23. Nitrini R, Lefèvre B, Mathias S, Caramelli P, Carrilho P, Sauaia N. Neuropsychological tests of simple application for diagnosing dementia. Arq Neuropsiquiatric. 1994;52(4):457–65.
24. Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, et al. International physical activity questionnaire (IPAQ): study of validity and reliability in Brazil. Rev Bras Ativ Fís Saúde. 2001;6(2):5–18.
25. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1-253.
26. Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, et al. Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement from the American College of Sports Medicine. Med Sci Sports Exerc. 2022;54(2):353–68.
27. Zhang Y, Yang Y, Huang Q, Zhang Q, Li M, Wu Y. The effectiveness of lifestyle interventions for diabetes remission on patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Worldviews Evid Based Nurs. 2023;20(1):64–78.
28. Zhu X, Zhao L, Chen J, Lin C, Lv F, Hu S, et al. The Effect of Physical Activity on Glycemic Variability in Patients With Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front Endocrinol (Lausanne). 2021; 12:767152.
29. Rietz M, Lehr A, Mino E, Lang A, Szczerba E, Schiemann T, et al. Physical Activity and Risk of Major Diabetes-Related Complications in Individuals With Diabetes: A Systematic Review and Meta-Analysis of Observational Studies. Diabetes Care. 2022;45(12):3101–11.
30. Ren C, Liu W, Li J, Cao Y, Xu J, Lu P. Physical activity and risk of diabetic retinopathy: a systematic review and meta-analysis. Acta Diabetol. 2019;56(8):823–37.
31. Botelho VH, Wendt A, Pinheiro E dos S, Crochemore-Silva I. Inequalities in sports and physical activity in the Brazilian macro-regions: PNAD, 2015. Rev Bras Ativ Fís Saúde. 2021;26:e0206.
32. Portela RA, Silva J, Nunes FF, Lopes M, Batista R, Silva A. Diabetes mellitus type 2: factors related to adherence to self-care. Rev Bras Enferm. 2022;75(4).
33. Santos P, Pereira R, Nakamura P, Moura R de. Factors that interfere with adhesion to the treatment of Diabetes Mellitus type 2. Res Soc Dev. 2022;11(1).
34. Santos IKS Dos, Conde WL. Bmi variation, dietary patterns and physical activity among adults aged 21-44 years. Cien Saude Colet. 2021;26:3853–63.
35. Gomes AC, Ribeiro GAM, Moraes MS, Gonçalves ICM, Sachett JAG. Adherence to pharmacological and nonpharmacological treatments in adults with type 2 diabetes. Mundo Saúde. 2020;44:381–96.
36. Santos AL, Marcon SS, Teston EF, Back IR, Lino IGT, Batista VC, et al. Adherence to the treatment of Diabetes mellitus and relationship with assistance in primary care. Reme Rev Min Enferm. 2020;24:e-1279.
37. Cartagena MV, Tort-Nasarre G, Arnaldo ER. Barriers and facilitators for physical activity in adults with type 2 diabetes mellitus: A scoping review. Int J Environ Res Public Health. 2021;18(10):5359.
38. Kolchraiber FC, Rocha JS, César DJ, Monteiro OO, Frederico GA, Gamba MA. Level of physical activity in people with type-2 diabetes mellitus. Rev Cuid. 2018;9(2):2105–16.
39. Silva AM, Fausto MCR, Gonçalves MJF. Care accessibility and availability for hypertensive patients in primary health care in a remote rural municipality in the state of Amazonas, Brazil, 2019. Cad Saude Publica. 2023;39(1):e00163722.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Lucas Santos Fernandes, Johrdy Amilton da Costa Braga, Maria Natália Cardoso, Tânia Rosane Bertoldo Benedetti, Hércules Lázaro Morais Campo, Elisa Brosina de Leon

This work is licensed under a Creative Commons Attribution 4.0 International License.
When submitting a manuscript to the Revista Brasileira de Atividade Física & Saúde, the authors retain the copyright to the article and authorize the Revista Brasileira de Atividade Física & Saúde to publish the manuscript under the Creative Commons Attribution 4.0 License and identify it as the original publication source.


