Arterial stiffness and leisure-time physical activity in community health workers: a cross-sectional study
DOI:
https://doi.org/10.12820/rbafs.29e0347Keywords:
Physical activity, Carotid-femoral pulse wave velocity, Primary Health Care, Healthcare professionalAbstract
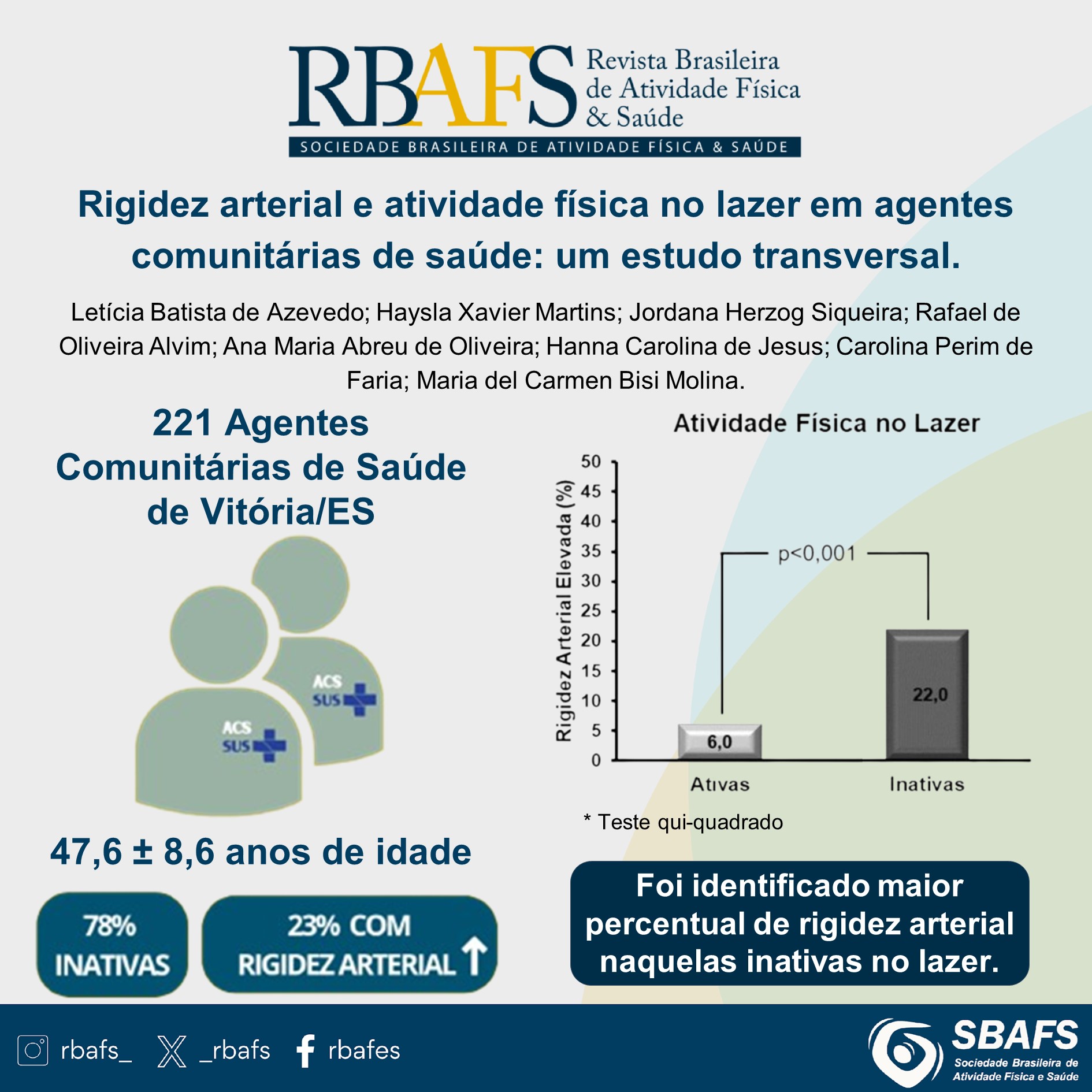
The high prevalences of non-communicable chronic diseases have been increasing in the population, including healthcare professionals, therefore, the association between leisure-time physical activity (LTPA) and arterial stiffness (AS) was evaluated through a cross-sectional study conducted with female community health agents (CHAs) from Vitória, Espírito Santo. LTPA was assessed using the international physical activity questionnaire, and AS was measured by carotid-femoral pulse wave velocity (cfPWV). Participants were considered active if they engaged in at least 150 minutes per week of moderate LTPA, 150 minutes per week of combined moderate and vigorous LTPA, or 75 minutes per week of vigorous LTPA. Elevated arterial stiffness was classified using a cut-off point of cfPWV ≥ the 90th percentile, stratified by sex and age group for a healthy population. Statistical tests were performed to compare proportions and means, with a p-value of <0.05 considered significant. A total of 221 CHAs (mean age 47.6 ± 8.6 years) were evaluated. Physical inactivity and elevated AS were observed in approximately 78% and 23% of the participants, respectively. A higher percentage of elevated AS was observed among CHAs who did not meet the LTPA recommendations (22.0%) compared to those who were physically active (6.0%) (p<0.001). Lower mean LTPA (15.6 ± 47.7 minutes per week) was observed among CHAs with elevated AS (p = 0.020). Physical inactivity is associated with elevated arterial stiffness. It is suggested that the promotion of LTPA be encouraged among professionals working on the front line of the Unified Health System, even if they perform work-related physical activities.
Downloads
References
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of Cardiovascular Events and All-Cause Mortality With Arterial Stiffness: A Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2010;55(13):1318–27. doi: https://doi.org/10.1016/j.jacc.2009.10.061. DOI: https://doi.org/10.1016/j.jacc.2009.10.061
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27(21):2588–605. doi: https://doi.org/10.1093/eurheartj/ehl254. DOI: https://doi.org/10.1093/eurheartj/ehl254
Park W, Park HY, Lim K, Park J. The role of habitual physical activity on arterial stiffness in elderly Individuals: a systematic review and meta-analysis. J Exerc Nutrition Biochem. 2017;21(4):16–21. doi: https://doi.org/10.20463/jenb.2017.0041. DOI: https://doi.org/10.20463/jenb.2017.16
Brasil. Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2021: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2021. Ministério da Saúde. Vol. 1. Brasília: Ministério da Saúde; 2021. 1–131 p. Disponível em: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/svsa/vigitel/vigitel-brasil-2021-estimativas-sobre-frequencia-e-distribuicao-sociodemografica-de-fatores-de-risco-e-protecao-para-doencas-cronicas/view. [22 Novembro].
Thompson PD, Buchner D, Piña IL, Balady GJ, Williams MA, Marcus BH, et al. Exercise and Physical Activity in the Prevention and Treatment of Atherosclerotic Cardiovascular Disease. Circulation. 2003;107(24):3109–16. doi: https://doi.org/10.1161/01.CIR.0000075572.40158.77. DOI: https://doi.org/10.1161/01.CIR.0000075572.40158.77
Lan YS, Khong TK, Yusof A. Effect of exercise on arterial stiffness in healthy young, middle-aged and older women: a systematic review. Nutrients. 2023;15(2):308. doi: https://doi.org/10.3390/nu15020308. DOI: https://doi.org/10.3390/nu15020308
Tanaka H, Dinenno FA, Monahan KD, Clevenger CM, DeSouza CA, Seals DR. Aging, Habitual Exercise, and Dynamic Arterial Compliance. Circulation. 2000;102(11):1270-5. doi: https://doi.org/10.1161/01.cir.102.11.1270. DOI: https://doi.org/10.1161/01.CIR.102.11.1270
Moreau K, Donato AJ, Seals DR, DeSouza CA, Tanaka H. Regular exercise, hormone replacement therapy and the age-related decline in carotid arterial compliance in healthy women. Cardiovasc Res. 2003;57(3):861–8. doi: https://doi.org/10.1016/s0008-6363(02)00777-0. DOI: https://doi.org/10.1016/S0008-6363(02)00777-0
Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de Atenção Básica. O trabalho do Agente Comunitário de Saúde. Série F Comunicação e Educação em Saúde. 2009;1:1–88.Disponível em: http://189.28.128.100/dab/docs/publicacoes/geral/manual_acs.pdf. [2022 Novembro].
Martins HX, Siqueira JH, de Oliveira AMA, de Jesus HC, Pereira TSS, Sichieri R, et al. Multimorbidade e cuidado com a saúde de agentes comunitários de saúde em Vitória, Espírito Santo, 2019: um estudo transversal. Epidemiol Serv Saúde. 2022;31(1). doi: http://dx.doi.org/10.1590/s1679-49742022000100006. DOI: https://doi.org/10.1590/s1679-49742022000100006
Paudel S, Subedi N, McLachlan CS, Smith BJ, Kallestrup P, Neupane D. Active commuting and leisure-time physical activity among adults in western Nepal: a cross-sectional study. BMJ Open. 2021;11(8):e051846. doi: https://doi.org/10.1136/bmjopen-2021-051846. DOI: https://doi.org/10.1136/bmjopen-2021-051846
Riaz H, Khan MS, Siddiqi TJ, Usman MS, Shah N, Goyal A, et al. Association Between Obesity and Cardiovascular Outcomes. JAMA Netw Open. 2018;1(7):e183788. doi: https://doi.org/10.1001/jamanetworkopen.2018.3788. DOI: https://doi.org/10.1001/jamanetworkopen.2018.3788
Nascimento BR, Brant LCC, Naback ADN, Veloso GA, Polanczyk CA, Ribeiro ALP, et al. Carga de Doenças Cardiovasculares Atribuível aos Fatores de Risco nos Países de Língua Portuguesa: Dados do Estudo “Global Burden of Disease 2019.” Arq Bras Cardiol. 2022;118(6):1028–48. doi: https://doi.org/10.36660/abc.20210680. DOI: https://doi.org/10.36660/abc.20210680
Molina MDCB, Martins HX, Siqueira JH, Oliveira AMA De, Jesus HC De, Pereira TSS. Impact of the training of community health workers on food education: methodological aspects and potentialities / Impacto da capacitação de agentes comunitários de saúde em educação alimentar: aspectos metodológicos e potencialidades. R pesq: cuid fundam online. 2021;13(1):1526–35. doi: https://doi.org/10.9789/2175-5361.rpcfo.v13.10266. DOI: https://doi.org/10.9789/2175-5361.rpcfo.v13.10266
Baldo MP, Cunha RS, Molina M del CB, Chór D, Griep RH, Duncan BB, et al. Carotid-femoral pulse wave velocity in a healthy adult sample: The ELSA-Brasil study. Int J Cardiol. 2018;15(251):90–5. doi: https://doi.org/10.1016/j.ijcard.2017.10.075. DOI: https://doi.org/10.1016/j.ijcard.2017.10.075
Associação Brasileira de Empresas de Pesquisas. Critério Brasil 2018 e atualização da distribuição de classes para 2018. São Paulo. 2018. p. 1-6. Disponível em: https://www.abep.org/criterio-brasil. [2022 Novembro].
Lohman TG. Anthropometric standardization reference manual. Champaign, IL.: Human Kinetics Books, Chicago, 1988.
World Health Organization. Obesity: preventing and managing the global epidemic: report of a WHO consultation. Geneva, Switzerland. World Health Organization, editor. Geneva: World Health Organization. 2000; 1–258 p. Disponível em: https://iris.who.int/handle/10665/42330. [2022 Novembro].
Lohman TJ, Roache AF, Martorell R. Anthropometric Standardization Reference Manual. Med Sci Sports Exerc. 1992;24(8):952. Disponível em: https://journals.lww.com/acsm-msse/citation/1992/08000/anthropometric_standardization_reference_manual.20.aspx. [2022 Novembro]. DOI: https://doi.org/10.1249/00005768-199208000-00020
Malachias MVB. 7th Brazilian Guideline of Arterial Hypertension: Presentation. Arq Bras Cardiol. 2016;107(3):0. doi: https://doi.org/10.5935/abc.20160140. DOI: https://doi.org/10.5935/abc.20160140
Golbert A, Vasques ACJ, Faria ACR de A, Lottenberg AMP, Joaquim AG, Vianna AGD, et al. Diretrizes da Sociedade Brasileira de Diabetes 2019-2020. São Paulo: Clannad; 2019. p. 1-491.
Faludi AA, Izar MCO, Saraiva JFK, Chacra APM, Bianco HT, Afiune A Neto, et al. Atualização da Diretriz Brasileira de Dislipidemias e Prevenção da Aterosclerose - 2017. Arq Bras Cardiol. 2017;109(2):1–76. doi: https://doi.org/10.5935/abc.20170121. DOI: https://doi.org/10.5935/abc.20170121
Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, et al. Questionário Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde. 2012;6(2):5-18.
World Health Organization. Mais pessoas ativas para um mundo mais saudável -Plano De Ação Global Para a Atividade Física 2018-2030: World Health Organization. 2018. Disponível em:www.who.int/lets-be-active/en/. [2022 Novembro].
Câmara SMA, Zunzunegui MV, Pirkle C, Moreira MA, Maciel ÁC. Menopausal status and physical performance in middle aged women: a cross-sectional community-based study in Northeast Brazil. PLoS One. 2015;10(3). doi: https://doi.org/10.1371/journal.pone.0119480. DOI: https://doi.org/10.1371/journal.pone.0119480
Lunz W, Molina MDCB, Rodrigues SLRL, Gonçalves CP, Baldo MP, Viana EC, et al. Impacto da atividade física sobre o risco cardiovascular na população adulta de Vitória-ES. Rev Bras Ciênc Mov. 2010;18(3):64-73.
Ballard AM, Davis A, Wong B, Lyn R, Thompson WR. The Effects of Exclusive Walking on Lipids and Lipoproteins in Women with Overweight and Obesity: A Systematic Review and Meta-Analysis. Am J Health Promot. 2022;36(2):328–39. doi: https://doi.org/10.1177/08901171211048135. DOI: https://doi.org/10.1177/08901171211048135
Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: an updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil. 2008;15(3):247-57. doi: https://doi.org/10.1097/HJR.0b013e3282f232ac. DOI: https://doi.org/10.1097/HJR.0b013e3282f232ac
Smith AD, Crippa A, Woodcock J, Brage S. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose–response meta-analysis of prospective cohort studies. Diabetologia. 2016;59(12):2527–45. doi: https://doi.org/10.1007/s00125-016-4079-0. DOI: https://doi.org/10.1007/s00125-016-4079-0
Boyer WR, Ehrlich SF, Crouter SE, Churilla JR, Fitzhugh EC. Leisure-time aerobic physical activity and the risk of diabetes-related mortality: An analysis of effect modification by race-ethnicity. J Diabetes Complications. 2021;35(1):107763. doi: https://doi.org/10.1016/j.jdiacomp.2020.107763. DOI: https://doi.org/10.1016/j.jdiacomp.2020.107763
Kelly S, Martin S, Kuhn I, Cowan A, Brayne C, Lafortune L. Barriers and Facilitators to the Uptake and Maintenance of Healthy Behaviours by People at Mid-Life: A Rapid Systematic Review. PLoS One. 2016;11(1):e0145074. doi: https://doi.org/10.1371/journal.pone.0145074. DOI: https://doi.org/10.1371/journal.pone.0145074
Galaviz KI, Harden SM, Smith E, Blackman KC, Berrey LM, Mama SK, et al. Physical activity promotion in Latin American populations: a systematic review on issues of internal and external validity. Int J Behav Nutr Phys Act. 2014;11(1):77. doi: https://doi.org/10.1186/1479-5868-11-77. DOI: https://doi.org/10.1186/1479-5868-11-77
Raza W, Krachler B, Forsberg B & Sommar JN. Health benefits of leisure time and commuting physical activity: A meta-analysis of effects on morbidity. J Transp Health. 2020;18:100873. doi: https://doi.org/10.1016/j.jth.2020.100873. DOI: https://doi.org/10.1016/j.jth.2020.100873
Otto CM. Heartbeat: Is all physical activity beneficial for cardiovascular health?. Heart. 2018;104(14):1137-1139. doi: https://doi.org/10.1136/heartjnl-2018-313725. DOI: https://doi.org/10.1136/heartjnl-2018-313725
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Leticia Batista de Azevedo, Haysla Xavier Martins, Jordana Herzog Siqueira, Rafael de Oliveira Alvim, Ana Maria Abreu de Oliveira, Hanna Carolina de Jesus, Carolina Perim de Faria, Maria del Carmen Bisi Molina

This work is licensed under a Creative Commons Attribution 4.0 International License.
When submitting a manuscript to the Revista Brasileira de Atividade Física & Saúde, the authors retain the copyright to the article and authorize the Revista Brasileira de Atividade Física & Saúde to publish the manuscript under the Creative Commons Attribution 4.0 License and identify it as the original publication source.


