Número de passos em diferentes dias da semana e horários na pandemia covid-19 em pessoas idosas com hipertensão arterial: Um estudo longitudinal
DOI:
https://doi.org/10.12820/rbafs.30e0417Palavras-chave:
Coronavírus, Envelhecimento, Atividade física, Comportamento sedentário, Fatores de riscoResumo
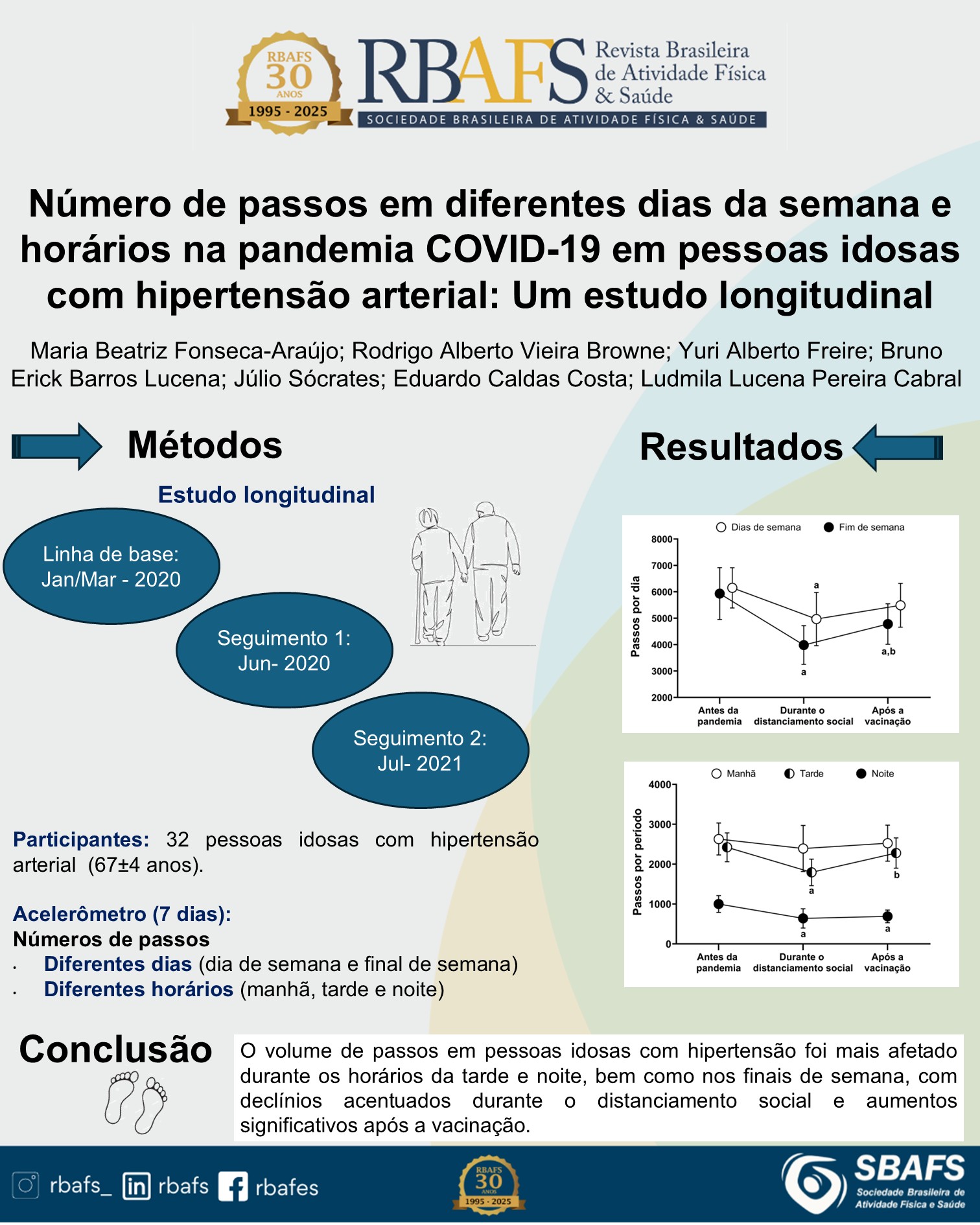
Objetivo: Foi analisar o número de passos em diferentes dias da semana e horários durante a pandemia covid-19 em pessoas idosas com hipertensão arterial. Métodos: Pessoas idosas com hipertensão arterial sem doenças cardiovasculares maiores (n = 32; 67 ± 4 anos) foram analisadas longitudinalmente (seguimento de 16-18 meses; pré-pandemia: janeiro/março-2020; distanciamento social: junho/2020; pós-vacinação: julho/2021). O número de passos foi mensurado por acelerometria (uma semana). Resultados: Houve diminuição do número de passos nos dias da semana e final de semana no distanciamento social (vs. pré-pandemia: β = 1.183 passos/dia; p = 0,018; β = 1.947 passos/dia; p < 0,001). Após vacinação, no final de semana, o número de passos permaneceu menor (vs. pré-pandemia: β = 1.152; p = 0,005), embora tenha aumentado pós-vacinação (vs. distanciamento social; β = 796; p < 0,027). Não houve mudança no horário da manhã (p > 0,05). No horário da tarde, houve diminuição no distanciamento social (vs. pré-pandemia: β = 629 passos/dia; p < 0,001), e aumento pós-vacinação (vs. distanciamento social: β = 485 passos/dia; p = 0,001). No horário da noite, houve diminuição no distanciamento social (vs. pré-pandemia: β = 360 passos/dia; p = 0,001) e pós-vacinação (vs. pré-pandemia: β = 310 passos/dia; p = 0,002). Conclusão: No distanciamento social, houve redução do número de passos na semana e final de semana, concentrada nos horários da tarde e noite. Ainda houve menor número de passos no horário da noite pós-vacinação, embora tenha se observado aumento nos finais de semana e horário da tarde em relação ao distanciamento social.
Downloads
Referências
1. Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157-60.
2. Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2021;64:108-10.
3. Katewongsa P, Widyastaria DA, Saonuam P, Haematulin N, Wongsingha N. The effects of the COVID-19 pandemic on the physical activity of the Thai population: Evidence from Thailand's Surveillance on Physical Activity 2020. J Sport Health Sci. 2021;10(3):341-348.
4. Browne RAV, Macêdo GAD, Cabral LLP, Oliveira GTA, Vivas A, Fontes EB, et al. Initial impact of the COVID-19 pandemic on physical activity and sedentary behavior in hypertensive older adults: An accelerometer-based analysis. Exp Gerontol. 2020;142:111121.
5. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-5.
6. Yamada Y, Namba H, Date H, Kitayama S, Nakayama Y, Kimura M, et al. Regional Difference in the Impact of COVID-19 Pandemic on Domain-Specific Physical Activity, Sedentary Behavior, Sleeping Time, and Step Count: Web-Based Cross-sectional Nationwide Survey and Accelerometer-Based Observational Study. JMIR Public Health Surveill. 2023;9:e39992.
7. Ataka T, Kimura N, Eguchi A, Matsubara E. Changes in objectively measured lifestyle factors during the COVID-19 pandemic in community-dwelling older adults. BMC Geriatr. 2022;22(1):326.
8. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al.Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):1583.
9. Dos Santos Ferreira Viero V, Matias TS, Alexandrino EG, Vieira YP, Meller FO, Schäfer AA, et al. Physical activity pattern before and during the COVID-19 pandemic and association with contextual variables of the pandemic in adults and older adults in southern Brazil. Z Gesundh Wiss. 2022:1-9.
10. Wu Z, Wang Y, Zhang Y, Bennell KL, White DK, Shen L, et al. The COVID-19 Pandemic and Daily Steps in the General Population: Meta-analysis of Observational Studies. JMIR Public Health Surveill. 2023;9:e40650.
11. Browne RAV, Cabral LLP, Freire YA, Macêdo GAD, Oliveira GTA, Vivas A, et al. Housing type is associated with objectively measured changes in movement behavior during the COVID-19 pandemic in older adults with hypertension: An exploratory study. Arch Gerontol Geriatr. 2021;94:104354.
12. Evenson KR, Buchner DM, Morland KB. Objective measurement of physical activity and sedentary behavior among US adults aged 60 years or older. Prev Chronic Dis. 2012;9:E26.
13. Sartini C, Wannamethee SG, Iliffe S, Morris RW, Ash S, Lennon L, et al. Diurnal patterns of objectively measured physical activity and sedentary behaviour in older men. BMC Public Health. 2015;15:609.
14. Arnardottir NY, Koster A, Van Domelen DR, Brychta RJ, Caserotti P, Eiriksdottir G, Sverrisdottir JE, Launer LJ, Gudnason V, Johannsson E, Harris TB, Chen KY, Sveinsson T. Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: Age, Gene/Environment Susceptibility-Reykjavik Study. Age Ageing. 2013 Mar;42(2):222-9.
15. Tudor-Locke C, Craig CL, Aoyagi Y, Bell RC, Croteau KA, De Bourdeaudhuij I, et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011;8:80.
16. Browne RAV, Cabral LLP, Oliveira GTA, Macêdo GAD, Sócrates J, Silva RM, et al. Life-Space Mobility and Objectively Measured Movement Behavior in Older Adults with Hypertension after Receiving COVID-19 Vaccination. Int J Environ Res Public Health. 2022;19(19):12532.
17. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Protocolos do Sistema de Vigilância Alimentar e Nutricional – SISVAN na assistência à saúde / Ministério da Saúde, Secretaria de Atenção à Saúde. Departamento de Atenção Básica.– Brasília : Ministério da Saúde, 2008. 61 p. : il.
18. Malachias MVB, Gomes MAM, Nobre F, Alessi A, Feitosa AD, Coelho EB. 7th Brazilian Guideline of Arterial Hypertension: Chapter 2 - Diagnosis and Classification. Arq Bras Cardiol. 2016;107(3 Suppl 3):7-13.
19. D'Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743-53.
20. American College of Sports Medicine; Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, Skinner JS. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510-30.
21. Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531-43.
22. Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357-64.
23. Perracini MR, de Amorim JSC, Lima CA, da Silva A, Trombini-Souza F, Pereira DS, et al. Impact of COVID-19 Pandemic on Life-Space Mobility of Older Adults Living in Brazil: REMOBILIZE Study. Front Public Health. 2021;9:643640.
24. Zając-Gawlak I, Pelclová J, Groffik D, Přidalová M, Nawrat-Szołtysik A, Kroemeke A, et al. Does physical activity lower the risk for metabolic syndrome: a longitudinal study of physically active older women. BMC Geriatr. 2021;21(1):11.
25. Cavero-Redondo I, Tudor-Locke C, Álvarez-Bueno C, Cunha PG, Aguiar EJ, Martínez-Vizcaíno V. Steps per Day and Arterial Stiffness. Hypertension. 2019;73(2):350-63.
26. Lee IM, Shiroma EJ, Kamada M, Bassett DR, Matthews CE, Buring JE. Association of Step Volume and Intensity With All-Cause Mortality in Older Women. JAMA Intern Med. 2019;179(8):1105-12.
27. Oikawa SY, Holloway TM, Phillips SM. The Impact of Step Reduction on Muscle Health in Aging: Protein and Exercise as Countermeasures. Front Nutr. 2019;6:75.
28. Brazil. Ministry of Health. Coronavirus disease case panel (COVID-19) in Brazil. Ministry of Health. Available from: <https://covid.saude.gov.br/> (2025 March).
29. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-20.
30. Schrack JA, Zipunnikov V, Goldsmith J, Bai J, Simonsick EM, Crainiceanu C, et al. Assessing the "physical cliff": detailed quantification of age-related differences in daily patterns of physical activity. J Gerontol A Biol Sci Med Sci. 2014;69(8):973-9.
31. Wheeler MJ, Dunstan DW, Ellis KA, Cerin E, Phillips S, Lambert G. Effect of Morning Exercise With or Without Breaks in Prolonged Sitting on Blood Pressure in Older Overweight/Obese Adults. Hypertension. 2019;73(4):859-67.
32. Paluch AE, Bajpai S, Bassett DR, Carnethon MR, Ekelund U, Evenson KR, et al. Daily steps and all-cause mortality: a meta-analysis of 15 international cohorts. Lancet Public Health. 2022;7(3):e219-e228.
Downloads
Publicado
Como Citar
Edição
Seção
Licença
Copyright (c) 2025 Maria Beatriz Fonseca-Araujo , Rodrigo Alberto Vieira Browne, Yuri Alberto Freire, Bruno Erick Barros Lucena, Júlio Sócrates, Eduardo Caldas Costa, Ludmila Lucena Pereira Cabral

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
Ao submeter um manuscrito à Revista Brasileira de Atividade Física & Saúde, os autores mantêm a titularidade dos direitos autorais sobre o artigo, e autorizam a Revista Brasileira de Atividade Física & Saúde a publicar esse manuscrito sob a Licença Creative Commons Atribuição 4.0 e identificá-la como veículo de sua publicação original.


