Atividade física para prevenir quedas em idosos: uma abordagem da Aotearoa Nova Zelândia
DOI:
https://doi.org/10.12820/rbafs.29e0366Palavras-chave:
Exercício, Prevenção de quedas, Força, EquilíbrioResumo
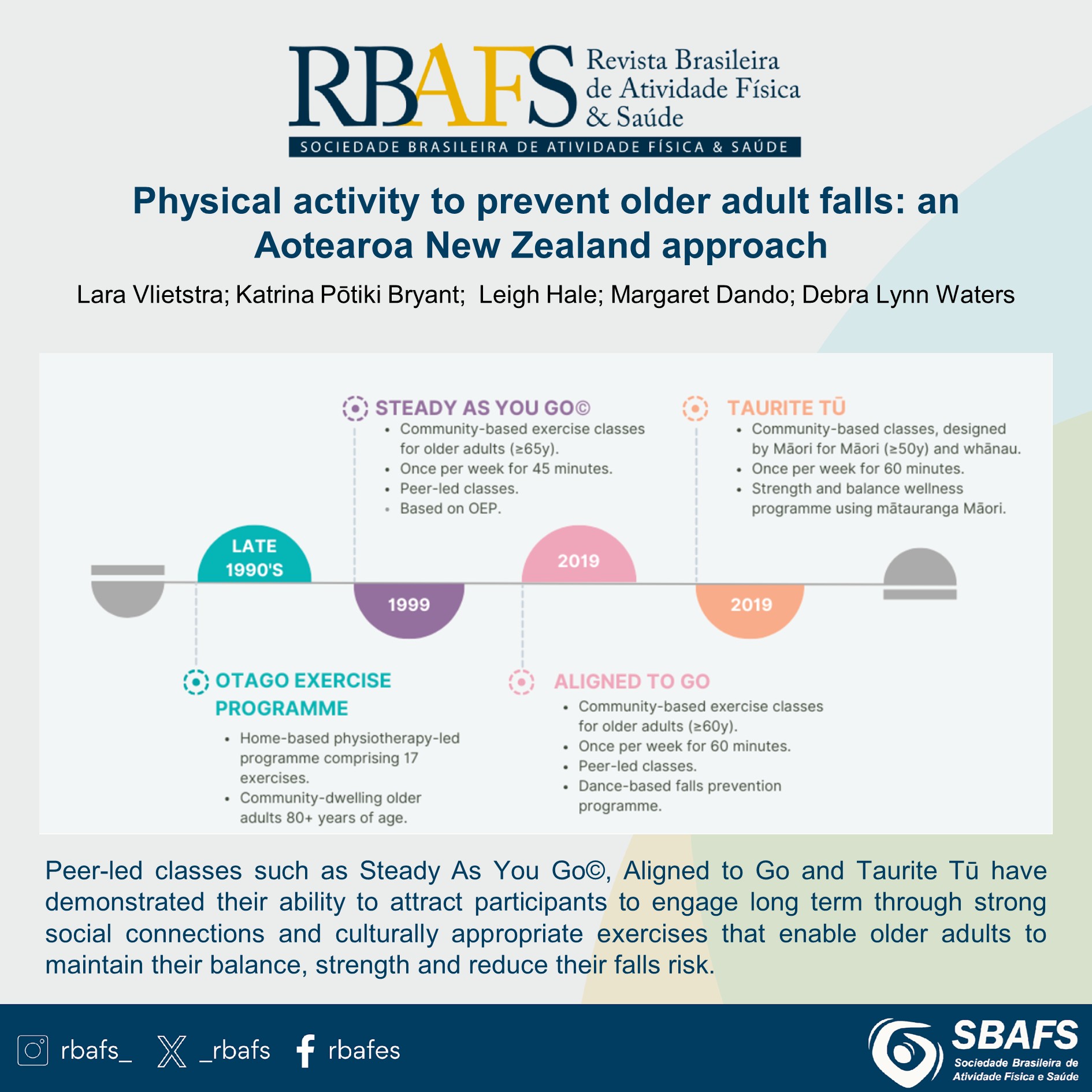
A atividade física e o exercício diminuem a incidência de quedas ao melhorar a marcha, o equilíbrio e a força. Todos os tipos de exercício, especialmente os exercícios funcionais e de equilíbrio, reduzem a taxa de quedas em aproximadamente 24%, a prática de caminhada isoladamente não reduz a incidência de quedas. A Nova Zelândia desenvolveu três programas de exercícios que têm se mostrado eficazes, estimuladores e sustentáveis para prevenção de quedas em pessoas idosas. O mundialmente renomado Programa de Exercícios Otago, realizado em casa, o Steady As You Go©, liderado por pares e baseado na comunidade, e o programa de exercícios indígenas Taurite Tū são exemplos desses programas. A maioria dos exercícios é realizada em pé e progride para que o participante fique com os pés juntos, em um pé só, minimizando o uso das mãos para ajudar no equilíbrio, e pratique movimentos controlados do centro de massa do corpo e da percepção corporal. As aulas lideradas por pares, como as dos programas Steady As You Go© e o Taurite Tū, demonstraram sua capacidade de atrair participantes para um envolvimento de longo prazo por meio de fortes conexões sociais e exercícios culturalmente apropriados, que permitem às pessoas idosas manter o equilíbrio, a força e reduzir o risco de quedas.
Downloads
Referências
Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One‐leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45(6):735-8. DOI: https://doi.org/10.1111/j.1532-5415.1997.tb01479.x
Gudnadottir M, Thorsteinsdottir TK, Mogensen B, Aspelund T, Thordardottir EB. Accidental injuries among older adults: An incidence study. Int. Emerg. Nurs. 2018;40:12-7. DOI: https://doi.org/10.1016/j.ienj.2018.03.003
Al-Aama T. Falls in the elderly: spectrum and prevention. Can fam physician Medecin de famille canadien. 2011;57(7):771-6.
Vasto S, Scapagnini G, Bulati M, Candore G, Castiglia L, Colonna-Romano G, et al. Biomarkes of aging. Front Biosci. (schol Ed). 2010;2:392-402. DOI: https://doi.org/10.2741/s72
Rodrigues F, Domingos C, Monteiro D, Morouço P. A review on aging, sarcopenia, falls, and resistance training in community-dwelling older adults. Int J Environ Res Public Health. 2022;19(2):874. DOI: https://doi.org/10.3390/ijerph19020874
Sun M, Min L, Xu N, Huang L, Li X. The Effect of Exercise Intervention on Reducing the Fall Risk in Older Adults: A Meta-Analysis of Randomized Controlled Trials. Int J Environ Res Public Health. 2021;18(23). DOI: https://doi.org/10.3390/ijerph182312562
Li F, Eckstrom E, Harmer P, Fitzgerald K, Voit J, Cameron KA. Exercise and fall prevention: Narrowing the research-to-practice gap and enhancing integration of clinical and community practice. J Am Geriatr Soc. 2016;64(2):425-31. DOI: https://doi.org/10.1111/jgs.13925
Sherrington C, Fairhall N, Kwok W, Wallbank G, Tiedemann A, Michaleff ZA, et al. Evidence on physical activity and falls prevention for people aged 65+ years: systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. Int J Behav Nutr Phys Act. 2020;17:144. DOI: https://doi.org/10.1186/s12966-020-01041-3
van Gameren M, Hoogendijk EO, van Schoor NM, Bossen D, Visser B, Bosmans JE, et al. Physical activity as a risk or protective factor for falls and fall-related fractures in non-frail and frail older adults: a longitudinal study. BMC Geriatr. 2022;22:695. DOI: https://doi.org/10.1186/s12877-022-03383-y
Gazibara T, Kurtagic I, Kisic-Tepavcevic D, Nurkovic S, Kovacevic N, Gazibara T, et al. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics. 2017;17(4):215-23. DOI: https://doi.org/10.1111/psyg.12217
Del Din S, Galna B, Lord S, Nieuwboer A, Bekkers EMJ, Pelosin E, et al. Falls Risk in Relation to Activity Exposure in High-Risk Older Adults. J Gerontol A Biol Sci Med Sci. 2020;75(6):1198-205. DOI: https://doi.org/10.1093/gerona/glaa007
Smith ML, Ory MG. Multi-directional nature of falls among older adults: A rationale for prevention and management. Front Public health. 2023;11. DOI: https://doi.org/10.3389/fpubh.2023.1117863
Lu Z, Lam FMH, Leung JCS, Kwok TCY. The U-Shaped Relationship Between Levels of Bouted Activity and Fall Incidence in Community-Dwelling Older Adults: A Prospective Cohort Study. J Gerontol Sci Med Sci. 2020;75 (10):e145-e151. DOI: https://doi.org/10.1093/gerona/glaa058
Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International ExerciseRecommendations in Older Adults (ICFSR): Expert consensus guidelines. J Nutr Health Aging. 2021;25(7):824-853. DOI: https://doi.org/10.1007/s12603-021-1665-8
Huang CY, Mayer PK, Wu MY, Liu DH, Wu PC, Yen HR. The effect of Tai Chi in elderly individuals with sarcopenia and frailty: A systematic review and meta-analysis of randomized controlled trials. Ageing Res Rev. 2022;82:101747. DOI: https://doi.org/10.1016/j.arr.2022.101747
Sherrington C, Tiedemann A, Fairhall N, Close JC, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W public Health Bull. 2011;22(3-4):78-83. DOI: https://doi.org/10.1071/NB10056
Shubert TE, Smith ML, Jiang L, Ory MG. Disseminating the Otago exercise program in the United States: Perceived and actual physical performance improvements from participants. J Appl Gerontol. 2018;37(1):79-98. DOI: https://doi.org/10.1177/0733464816675422
Campbell AJ, Robertson MC. Otago Exercise Programme to prevent falls in older adults: A home-based, individually tailored strength and balance retraining programme Otago; 2003.
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–9. DOI: https://doi.org/10.1136/bmj.315.7115.1065
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: A randomized, controlled trial. J Am Geriatr Soc. 1999;47(7):850-3. DOI: https://doi.org/10.1111/j.1532-5415.1999.tb03843.x
Martins AC, Santos C, Silva C, Baltazar D, Moreira J, Tavares N. Does modified Otago Exercise Program improves balance in older people? A systematic review. Prev Med Rep. 2018;11:231-9. DOI: https://doi.org/10.1016/j.pmedr.2018.06.015
Thomas S, Mackintosh S, Halbert J. Does the 'Otago exercise programme' reduce mortality and falls in older adults?: a systematic review and meta-analysis. Age Ageing. 2010;39(6):681-7. DOI: https://doi.org/10.1093/ageing/afq102
Yi M, Zhang W, Zhang X, Zhou J, Wang Z. The effectiveness of Otago exercise program in older adults with frailty or pre-frailty: A systematic review and meta-analysis. Arch Gerontol Geriatr. 2023;114:105083. DOI: https://doi.org/10.1016/j.archger.2023.105083
Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-8. DOI: https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
Omaña H, Bezaire K, Brady K, Davies J, Louwagie N, Power S, et al. Functional Reach Test, Single-Leg Stance Test, and Tinetti Performance-Oriented Mobility Assessment for the Prediction of Falls in Older Adults: A Systematic Review. Phys Ther. 2021;101(10):pzab173. DOI: https://doi.org/10.1093/ptj/pzab173
Bohannon RW. Reference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from elders. Percept Mot Skills. 2006;103(1):215-22. DOI: https://doi.org/10.2466/pms.103.1.215-222
Waters DL, Hale LA, Robertson L, Hale BA, Herbison P. Evaluation of a peer-led falls prevention program for older adults. Arch Phys Med Rehabil. 2011;92(10):1581-6. DOI: https://doi.org/10.1016/j.apmr.2011.05.014
Wu S, Guo Y, Cao Z, Nan J, Zhang Q, Hu M, et al. Effects of Otago exercise program on physical function in older adults: A systematic review and meta-analysis of randomized controlled trials. Arch Gerontol Geriatr. 2024;124:105470. DOI: https://doi.org/10.1016/j.archger.2024.105470
Lesinski M, Hortobágyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of Balance Training on Balance Performance in Healthy Older Adults: A Systematic Review and Meta-analysis. Sports Med. 2015;45(12):1721-38. DOI: https://doi.org/10.1007/s40279-015-0375-y
Theou O, Stathokostas L, Roland KP, Jakobi JM, Patterson C, Vandervoort AA, et al. The effectiveness of exercise interventions for the management of frailty: a systematic review. J Aging Res. 2011;2011:569194. DOI: https://doi.org/10.4061/2011/569194
Chaabene H, Prieske O, Herz M, Moran J, Höhne J, Kliegl R, et al. Home-based exercise programmes improve physical fitness of healthy older adults: A PRISMA-compliant systematic review and meta-analysis with relevance for COVID-19. Ageing Res Rev. 2021. 67:101265. DOI: https://doi.org/10.1016/j.arr.2021.101265
Wurzer B, Waters DL, Hale LA, Leon de la Barra S. Long-term participation in peer-led fall prevention classes predicts lower fall incidence. Arch Phys med rehabil. 2014;95(6):1060-6. DOI: https://doi.org/10.1016/j.apmr.2014.01.018
Wurzer B, Waters DL, Hale LA. Fall-Related Injuries in a Cohort of Community-Dwelling Older Adults Attending Peer-Led Fall Prevention Exercise Classes. J Geriatr Phys Ther. 2016;39(3):110-6. DOI: https://doi.org/10.1519/JPT.0000000000000061
Robertson L, Hale B, Hale L, Waters DL. A qualitative study of community peer-led exercise groups, their wellbeing and social effects. Int J Allied Health Sci Pract. 2014;12(2). DOI: https://doi.org/10.46743/1540-580X/2014.1483
Robertson LJ, Hale BA, Waters DL. Peer leaders as volunteers: Their role in sustain-able community groups. Gerontechnology. 2016;15(suppl):58s.
Smith J, Whittington F, Ackermann C, Clarke R, Hoten-Walker G, Kubba Y, et al. Impact of the 2020 New Zealand COVID-19 lockdown on participants in a community-based, peer-led fall prevention program. Australasian J ageing. 2022;41(3):e240-e248. DOI: https://doi.org/10.1111/ajag.13040
Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297(1):77-86. DOI: https://doi.org/10.1001/jama.297.1.77
Peeters G, Dobson AJ, Deeg DJ, Brown WJ. A life-course perspective on physical functioning in women. Bull World Health Organ. 2013;91(9):661-70. DOI: https://doi.org/10.2471/BLT.13.123075
Bryant KP. Taurite Tū, achieving equitable injury prevention outcomes for ageing Māori. 2023. Available in: <https://www.tauritetu.co.nz/media/3brisymb/research-report.pdf> [2024 june]
Lord SR, Close JCT. New horizons in falls prevention. Age Ageing. 2018;47(4):492-8. DOI: https://doi.org/10.1093/ageing/afy059
Hale L, Higgs C, Keen D, Smith C. It Is "All About Relationships" in Lifestyle Programmes for Adults Living With Type Two Diabetes Underpinned by a Person/Whānau-Centred Care Approach. Front Rehabil Sci 2022;3:829542. DOI: https://doi.org/10.3389/fresc.2022.829542
Downloads
Publicado
Como Citar
Edição
Seção
Licença
Copyright (c) 2024 Lara Vlietstra, Katrina Pōtiki Bryant, Leigh Hale, Margaret Dando, Debra Waters

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
Ao submeter um manuscrito à Revista Brasileira de Atividade Física & Saúde, os autores mantêm a titularidade dos direitos autorais sobre o artigo, e autorizam a Revista Brasileira de Atividade Física & Saúde a publicar esse manuscrito sob a Licença Creative Commons Atribuição 4.0 e identificá-la como veículo de sua publicação original.


